“Pendevice Therapy – A Game Changer”
World Haemophilia Day

DR K.K KOUL
World Haemophilia Day (WHD) is observed annually on april 17th to commemorate the birth day of Frank Schnabel, who founded the World Federation of Haemophilia (WFH). This occasion serves as a platform to increase awareness & provide education about Haemophilia A (HA), Haemophilia B (HB), vonwillibrand disease & other bleeding disorders. The WFH encourages people worldwide to illuminate in red as a symbol of solidarity with those affected by Haemophilia. The theme for WHD 2024 is “Equitable Access for All : Recognising all bleeding Disorders”. The etymological definition of Haemophilia is Love of blood – name suggested by a medical treatise in 1828. Two Greek words – haima (meaning blood) & philia (meaning affection (attraction to blood) are the origin for the term Haemophilia.

Haemophilias are largely a group of Disorders of Bleeding caused by genetic mutation in the sex chromosome – X, resulting in functional loss for the quantitative or qualitative abnormalities in either clotting factor VIII (F8) or clotting factor IX (F9), thereby segregating the two into Haemophilia – A (HA) and Haemophilia – B (HB) respectively. This defect is estimated to occur 1 in 5000 live male birth for HA and 1 in 20,000 live male birth for HB & often runs in families. However about a third of cases develop amongst healthy families from the denovo mutation. Haemophilia generally affects males (XY) on the maternal side. Girls (XX) are generally resistant to clinical fury of Haemophilia & lead symptom free life.
Since different bleeding disorders may have very similar symptoms ; therefore, accurate diagnosis is essential to ensure appropriate management. Haemophilia presents with a history of easy bruising in early childhood, spontaneous bleeding particularly into large joints, muscles and soft tissues. Life threatening bleeds (Head and Neck and other internal bleeds), excessive bleeding following trauma or surgery. People with Haemophilia (PwH) have no or low levels of clotting factor VIII (F8) in HA or F9 in HB & therefore low thrombin generation & thus blood cannot effectively clot. There is imbalance between clotting factors (either absent or low levels) and natural anticoagulation factors (which are plentiful) and thus thrombin generation is very low.
Drug Products Available for Haemophilia : Clotting Factor Therapy (CFT) – Blood plasma derived (pd) Standard half – life (pdSHL) and recombinant technology based SHL (rtSHL) & recombinant extended half life (rtEHL) products. Bypassing Agents for PwH with inhibitors : Activated Prothrombin Complex Concentrate (aPCC, Feiba) & Recombinant activated factor VII (rtF VIIa, Novoseven). Non clotting factor therapy (NFT) – Emicizumab (Hemlibra) (FVIII Mimetic) is a recombinant bispecific momoclonal EHL drug product for prophylactic use once in a month by subcutaneous infusion for Haemophilia A with or without inhibitors. At present this has very high percentage of compliance and adherence by the HA patients. NFT EHL products are not yet available for Haemophilia B
Emerging Therapies : The potential new products include
a) improved factor products ( EHL & delivery by subcutaneous injection )
b) Haemostatic rebalancing agents c) Gene Therapy & Genome editing therapy – Gene therapy refers to the addition of New genes to human cells, while genome editing involves the precise manipulation of specific sequence of the human genome for disease management. Gene therapy for Haemophilia B has been approved for use in USA. Trial for Gene therapy for Haemophilia A has recently been started on one patient at CMC Vellore (India)
Haemostatic rebalancing agents (HRBA) – these mainly reduce or inhibit the activity of anticoagulants (Anti thrombin, Tissue factor pathway inhibitor (TFPI), Activated protein C) in the system thereby restoring the balance and thus increase thrombin generation which restores Haemostasis. Hence it is used in both HA & HB with or without inhibitors. HRBA include – a) Fitusiran which specifically targets antithrombin mRNA leading to suppression of antithrombin in the Liver b) Anti-TFPI antibodies represent another modality in clinical trials. Two anti-TFPI (Concizumab & Marstacimab) clinical programs are ongoing while two others have seen evidence of thrombotic complications. Concizumab has been approved for use in Canada for HB patients with inhibitors. It shall be available in India aswell after couple of months for use in HA and HB patients with or without inhibitors.
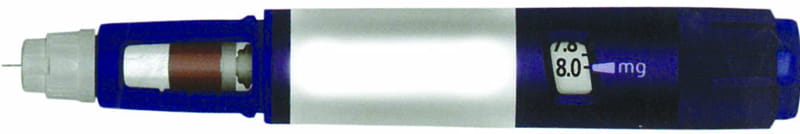
Pen devices in haemophilia : a gamechanger towards a better future for a person with hemophilia
Adherence to haemophilia treatment significantly affects clinical outcomes and quality of life. In the present haemophilia era of vial formulations, some of the major limitations to treatment adherence are the time spent in reconstitution and administration, injection volume and drug wastage, pain and lack of self-infusion capability. Long-term administration of such treatment options can lead to inconvenience, discomfort or pain, thereby reducing patient adherence. Although pen devices are not new and are widely used in other chronic conditions such as diabetes and growth disorders, their adoption in haemophilia care is a crucial unmet need. The introduction of pen devices is essential to enhance treatment adherence in hemophilia, offering a more convenient and comfortable administration experience. Moreover, the use of smaller needles can lead to reduced pain and bleeding, contributing to a less traumatic and painless injection experience. In addition to the device features, it would be beneficial if the pen could be flexible to be used for all hemophilia subtypes (HA and HB with/without inhibitors) and allow for storage at both refrigeration and room temperatures.
In summary, the ease of administration in haemophilia care is often overlooked but is an important aspect that needs to be considered among the characteristics of an ideal treatment option. The future integration of pen devices has the potential to simplify administration, enhance user-friendliness, reduce injection-associated pain, and increase confidence in use. Access to such pen devices within the hemophilia community has the potential to be transformative, presenting a significant improvement in the healthcare experience for individuals with hemophilia. Pen devices in haemophilia is indeed going to be a boon and definitely a game changer in empowering a person with haemophilia.
(The writer is President HHCN ; Former Prof. & Head Pathology, GMC Jammu).
